
Should Healthcare Practitioners Have More Power in the Health Policy-making Process?
April 15, 2015
Deep Brain Stimulation for the treatment of Obsessive Compulsive Disorder
July 26, 2015“A focus on quality helps to ensure that scarce resources are used in an efficient and effective way. Without quality there will be no trust in the effectiveness of the system.” WHO
The Concept of Quality
Before going into more detail about how quality can be improved, I believe it is important to first define quality and then explore how it has evolved over time. One of the first definitions of quality in health care appearing in medical literature is that by Lee and Jones (1933) who define quality of care as “a matter of judgments with respect to certain aspects, properties, ingredients or dimensions of a process called health service”. Since then, various individuals as well as health organisations have tried to define quality, with varying degrees of success; the concept of quality in health care involves considerable complexity (Donabedian, 1980).
I believe that the best definition should be one that takes into account the three main actors in every health care system: patients, healthcare organisations and funding agencies. A definition including all three is found in the work of Paccaud (1993) who states that quality is the complete satisfaction of those most in need of care, according to the professional knowledge of the moment, at the lowest possible cost to the health organisation and within the limits set by the health authorities and by those who are called upon to pay.
Quality in the Context of Mental Health
Since the late nineties, clinical improvement has not remained the sole focus of psychiatric interventions, with greater importance given also to maximising the patient’s functioning and general wellbeing by taking into account their preferences and needs. The assessment of quality of care has now become a key element in the organisation of modern day psychiatric hospitals (Garety, et al., 2006). Quality of care provided by a psychiatric hospital is a multidimensional concept, related to structural as well as organisational aspects, which are both critical factors in the provision of health care services (Pincus, et al., 2007), and can be examined either from an ‘objective’ (healthcare practitioners, policy makers and service providers) or ‘subjective’ (mental health users, their families and friends, and the general population) point of view.
So why is it important to define quality in the context of Mental Health? According to the Mental Health Policy and Service Guidance Package (WHO, 2003): “Quality is important for all mental health systems, from a variety of perspectives. From the perspective of a person with a mental disorder, quality ensures that they receive the care they require and their symptoms and quality of life improve. From the perspective of a family member, quality provides support and helps preserve family integrity. From the perspective of a service provider or programme manager, quality ensures effectiveness and efficiency. From the perspective of a policy maker, quality is the key to improving the mental health of the population, ensuring value for monies expended and accountability.”
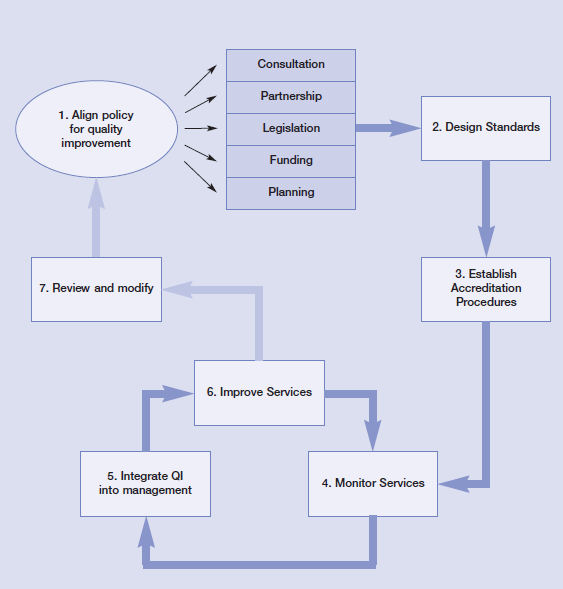
The WHO package includes a step-by-step approach for the creation of a programme which is meant to provide countries with a structure in order to improve the quality of mental health care. Since the organisation I work for is at the core of Malta’s mental health service provision, I will be using the guideline in order to outline how quality can be improved. There are seven steps in the program. These are: align policy for quality improvement; design a standards document; establish accreditation procedures, monitor the mental health service by using the quality mechanisms; integrate quality improvement into the on-going management and delivery of services; consider systematic reform for the improvement of services; and review the quality mechanisms (World Heath Organization, 2003). These steps are cyclical in nature and are represented in the figure below
Aligning Policy for Quality Improvement
“Mental health policies have to be aligned so that they support rather than oppose the improvement of quality.” (WHO)
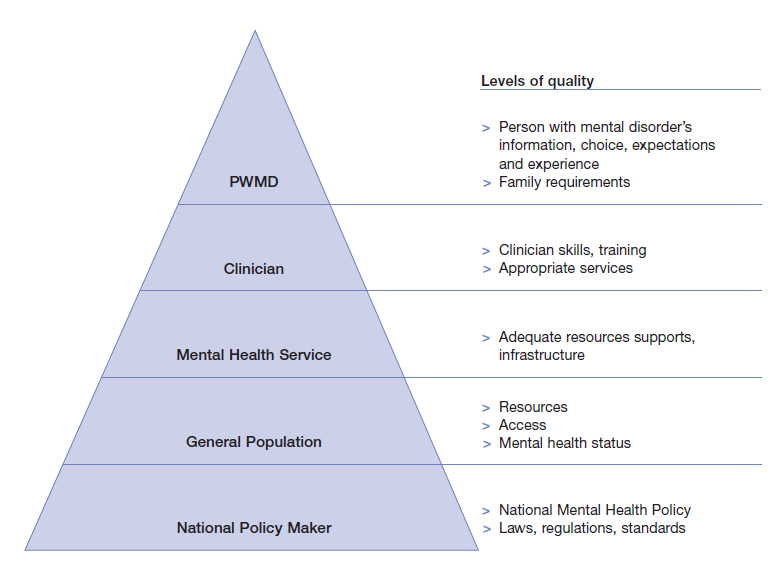
The first task that needs to be undertaken is the creation of a vision of quality that is common to all stakeholders, including policy-makers and policy funders, mental healthcare workers, psychiatric patients and their family members. This is not an easy task, as stakeholders may have dissimilar needs; creating different levels of quality, as can be seen in the figure below:
Another important factor that must be taken into consideration is that whilst much progress has been made with respect to national health policy, especially over the last two decades (since the 1987 Labour electoral defeat and subsequent successive Nationalist legislations), mental health policy has notoriously lagged behind (Health Information Unit, 2001). There are a number of reasons for this, but the most likely is the stigma that has long plagued psychiatry in Malta and Mount Carmel Hospital in particular (Massa, 2009; Aquilina, 2012).
Despite the challenges that are undoubtedly present, policy makers, in collaboration with the hospital’s management, need to establish, through a consultation process, the quality parameters being sought. Consultation is arguably the most important of these parameters, not only in the alignment of policy for quality improvement but throughout the other steps of the program. For this to be effective, I believe there needs to be a radical change in mentality. This would involve setting aside the prevalent paternalistic and custodial culture to create one that values and rewards performance and quality. This can only be done if the management look beyond the hospital’s 19th century walls and reach out to the various stakeholders that exist.
Designing a standards document
“An essential step towards improving the quality of mental health services is to set out a formal measurable description of the way in which care should be delivered.” (WHO, 2003)
Whilst many countries have taken this crucial step for improving quality of care (National Standards for Mental Health Services, 1997; National service framework for mental health: modern standards and service models, 1999; Quality standard for service user experience in adult mental health, 2012), unfortunately, no formal standards document has been produced for the mental health services offered by Mount Carmel Hospital, which instead relies on the expertise of its consultants in a scenario more akin to the wild west. This has historically led to much confusion and certainly much friction between different consultant-led firms, in an inevitable clash of egos.
I believe that the root cause of this is the lack of a standards document which would clearly outline the gold standard of clinical practise to which all firms would need to adhere to. This would not entail a re-invention of the wheel, but rather an adaptation of internationally recognised standards to the local scenario. The Clinical Chairperson of Psychiatry, who has direct responsibility for clinical practise, should set up a working group or special committee composed of representatives from the major stakeholders, including the hospital’s management (the board of directors, the CEO, the financial controller, the principal administration and the operations managers), healthcare providers (psychiatrists, psychiatric trainees, nurses, occupational therapists, psychologists, social workers, physiotherapists, pharmacists, and laboratory services), community services (outpatient team, roaming team, outreach team, crisis intervention team and volunteer services), as well as patient’s and relative’s associations (Malta Mental Health association). The aim should be that of auditing current practise in order to create a set of standards which reflect contemporary best-psychiatric practise whilst encompassing the hospital’s mission statement and reaching a compromise between the interests and needs of the various stakeholders involved. Since the Maltese National Health Service follows closely that of the UK, I believe that inspiration could be drawn from the Royal College of Psychiatrists accreditation procedure (2010), which sets the standards for in-patient care in psychiatric ward settings.
Establishing accreditation procedures
“Accreditation is the official authorization of a mental health service by a public body that is legally entitled to fulfil this role. In the context of quality, accreditation has come to mean the authorization of a service on condition that certain criteria of quality are demonstrably met.” (WHO, 2003)
Accreditation should be an essential requirement for the operation of a hospital, ensuring monitoring of performance levels in relation to previously established standards whilst striving to continuously improve quality of care provided (Rawlins, 2001). Mount Carmel Hospital lacks any form of accreditation procedures and therefore this process needs to be drawn from the ground up, again through consultation with all the relevant stakeholders. These procedures should be based upon established standards of care (see previous sub-heading) and take into account the needs of all parties involved. In order to achieve increased transparency, I believe that the functioning and financing of the hospital’s accreditation procedure should be independent from the department of health. Unfortunately, in order for this to take place, it is likely that a foreign company (such as QHA Trent, UK or La Haute Autorité de santé, France) would need to be enlisted, as such services are not offered locally, resulting in a greater overall expense.
Monitoring mental health service by using quality mechanisms
“Services should be monitored and assessed on a regular basis in accordance with the agreed standards and accreditation procedures.” (WHO, 2003)
Once standards and accreditation procedures have been put in place, it is important to find an appropriate method by which quality of care can be monitored. Over the years, health quality measurements have been developed in order to aid in the analysis of care provided, with the goal of increasing efficiency. It is imperative that these measurements are reproducible, generalizable and have a strong scientific basis (McGlynn, 1998). Measurements of quality include: evidence based medicine, the Balanced Scorecard system, patient satisfaction, service lists, etc. These tools provide a litmus test through which the quality of the healthcare organisation can be assessed, and once areas of weakness have been identified, improved. I strongly believe that this is one of the most important steps in improving the quality of healthcare at Mount Carmel Hospital
An essential element of monitoring the quality of mental health services is the use of a motivational approach to improve quality. From personal experience working at Mount Carmel Hospital, I would have to state that, unfortunately, there is a strong culture of blame. I would go so far as to say that it is not only a culture of blame but a culture of fear. The hospital’s health practitioners rarely communicate their mistakes to their patients and even less so to the health authorities for fear of litigation, leading to a form of medical practise known as defensive medicine. I believe that there needs to be a change in mentality, with a shift from the culture of blame to what has become known as a “just culture”. This is not an easy process, as the damage caused by decades of culture of blame is difficult to overcome. However, I believe one should learn from mistakes, even those that occur in health care; as long as health practitioners are treated like fiends, after committing even the slightest mistake, one cannot expect an accurate and reliable system for the reporting of errors and therefore preventing the recurrence of adverse events.
The hospital should embark on a multi-prong approach to measuring the quality of its mental health services. I believe a good place to begin is deciding on quality indicators for benchmarking the level of care. A number of studies (Hermann, et al., 2006; Druss, Rosenheck, & Stolar, 1999; Shield, et al., 2003) have already identified the most important indicators with respect to mental health. However, in a country like Malta, which has minimal mental health resources, the mobilisation of financial backing and personal needed to carry out this exercise may be difficult. This is where the issue of prioritisation takes the centre stage; the most affordable and practical indicators therefore need to be selected. One of the most widely accepted frameworks for prioritisation is Cost Effectiveness Analysis (Drummond, Sculpher, Torrance, O' Brien, & Stoddart, 2005) that compares the cost and effects of two or more courses of action.
With respect to Mount Carmel Hospital, I believe that indicators which may be drawn from pre-existing data that the hospital collects as part of routine care, should be used; these are practical to measure and do not pose a strain on financial resources. They include: the number of psychiatrist and/or psychotherapist visits during the acute phase of treatment (Veterans Health Administration, 2000); number of hospital readmissions (Pirkis, Burgess, Dunt, & Henry, 1999); the use of psychotropic medications with anticholinergic effect in elderly patients (Wells, et al., 1994); the number of persons followed up by a mental health practitioner soon after discharge (McEwan & Goldner, 2001); the number of patients with severe psychiatric disorder who receive case management (McEwan & Goldner, 2001); and the standardised mortality rate for patients suffering from psychiatric disorders (McEwan & Goldner, 2001). These indicators measure processes and outcomes which are clinically important in the sphere of quality in clinical practice and may also be useful in “identifying consensus-based measures for international benchmarking of mental health care.” (Hermann, et al., 2006)
Integrating quality improvement into the on-going management and delivery of services
“Once mechanisms are in place for assessing the quality of local mental health care (through standards, accreditation procedures and monitoring systems), continuous quality improvement should be built into the management and delivery of services.” (WHO, 2003)
This process can also be termed Quality Management, which is the part of health care management that deals with the improvement of performance during production or delivery of the health service instead of trying to fix problems after the final product has been produced (James, 1989). A good model (Langley, Nolan, Nolan, Norman, & Provost, 2009) for quality improvement incorporates a number of steps: “planning a change; trying it; observing the results; and acting on what has been learnt.”
There are a number of methods (World Heath Organization, 2003) by which mental health care of optimal quality can be continuously provided. These include: the use of service quality reviews; checking quality, improving quality in clinical practise (evidence based medicine, clinical guidelines, continued professional development); and auditing. A number of these processes are carried out frequently at Mount Carmel Hospital. These include audits, financial as well as clinical, and continued professional development. Whilst most psychiatric consultants and trainees are up to date with the latest guidelines most widely used in psychiatry, including those produced by National Institute for Health and Clinical Excellence, the Royal College of Psychiatrists and the American Psychiatric Association, Mount Carmel Hospital has rarely produced any clinical guidelines of its own. This would be important in aligning care and ensuring that the most up-to-date evidence based psychiatry is in place to offer the highest level of quality in the delivery of mental health services.
Systematic reform for the improvement of services - A Conclusion
“In addition to the on-going management and continuous improvement of the quality of services, the assessment of a mental health service may highlight a need for a systematic reform or improvement of services. This step may require concerted planning and coordination by various sectors.” (WHO, 2003)
Having reviewed the main areas where quality needs to be improved in the delivery of psychiatry in Malta, it becomes manifestly obvious that a drastic, widespread and systematic reform is needed in order to ensure that the hospital indeed provides a level of health care that it sets out in its mission statement (Mental Health Services, 2011). I believe that the main emphasis of this large-scale reform should be the transfer of services from the century’s old institutional care to community-based care, a transformation that has occurred in most western health care systems; literature (Jones, 1989; Goodwin, 1997) has consistently shown that quality of care is improved when patients are offered community based care when compared to institutional care.
Locally, following a pilot project in 1994 to establish community services for a population of 35,000 persons (Malta has a population of 420,000) the community services have been extended to six regions in Malta, covering a total of 198,000 persons. The effort is to be commended: psychiatrists now have the opportunity to provide assessments and management within a more personalised and sub culturally sensitive setting, working within a team of professionals, providing pharmacological and psychotherapeutic interventions, as well as a leadership role of the multidisciplinary team. However, this extension of services has had a negative impact; resources have been stretched to the absolute limit, with healthcare providers being obliged to provide community services with little in terms of recruitment of further manpower.
This current point in time reflects an important transition period for Maltese psychiatry, where the institutional framework for the provision of community services is being setup and strengthened. This process is not without its challenges and unfortunately, I believe that the move to community based services has been a case of ‘trying to run before learning how to walk’. Due to the fact that a large-scale reform is needed, the hospital’s management should adopt a system approach, which has been shown to be beneficial in such scenarios (Thornicroft & Tansella, 1999) in order to ensure a high level of quality in the provision of mental health services.

